Fractures of the Fifth Metatarsal

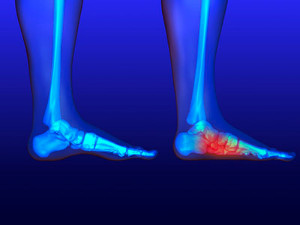
A 5th metatarsal fracture involves a break in the long bone on the outer side of the foot, often caused by a sudden twist, direct impact, or overuse. This type of fracture is common in athletes and active individuals. Symptoms typically include sharp pain on the outside of the foot, swelling, bruising, and difficulty walking or bearing weight. Treatment for a fifth metatarsal fracture depends on the severity of the break. For minor fractures, rest might be sufficient, along with protective footwear or a walking boot. However, more severe fractures may require immobilization with a cast or even surgical intervention to properly align the bone. If you suspect a fifth metatarsal fracture, it is important to seek medical attention to prevent complications and ensure proper healing. It is suggested you schedule an appointment with a podiatrist for a comprehensive evaluation and tailored treatment plan to get you back on your feet.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Dr. Steven Shlonsky from Louisville, Kentucky. Dr. Shlonsky can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Louisville, KY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Erythromelalgia and Its Impact on the Feet

Erythromelalgia is a rare condition marked by severe burning pain, redness, and heat in the extremities, particularly affecting the feet. Individuals often experience debilitating symptoms that flare up in response to heat, exertion, or prolonged standing, leading to significant discomfort. The exact cause of erythromelalgia is not fully understood, but it is thought to involve abnormalities in blood flow and nerve function. This condition can affect people of all ages, but it is more commonly observed in adults, especially women. In the feet, erythromelalgia can hinder mobility and impact daily activities, making even simple tasks challenging. Understanding erythromelalgia is vital for those affected, as timely diagnosis and appropriate management strategies can help alleviate symptoms and improve overall quality of life. If you have any of the above symptoms, it is strongly suggested that you promptly consult a podiatrist who can help you to manage this condition.
Some foot conditions may require additional professional care. If you have any concerns, contact Dr. Steven Shlonsky of Louisville, Kentucky. Dr. Shlonsky can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Louisville, KY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
Is My Toe Broken?

A broken toe can cause significant discomfort and disrupt daily activities. Common symptoms include intense pain at the site of injury, swelling, bruising, and difficulty walking. The toe may appear deformed or misaligned, and there can be tenderness when touched. Various factors contribute to broken toes, with osteoporosis being a notable cause. This condition weakens bones, making them more susceptible to fractures. Stress fractures, which occur from repetitive impact or overuse, can also lead to breaks in the toe. Additionally, dropping a heavy object on the foot is a frequent cause of toe fractures. There are various treatment methods for a broken toe, depending on the severity of the fracture. If you have broken your toe, it is suggested that you consult a podiatrist who can treat it effectively.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Dr. Steven Shlonsky from Louisville, Kentucky. Dr. Shlonsky will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Louisville, KY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Facts About Flat Feet
Pes planus, commonly known as flat feet, is caused by the loss of the medial longitudinal arch of the foot. This results in the entire sole making contact with the ground, leading to a flat appearance. Various factors contribute to the development of pes planus. Genetic predisposition plays a significant role, as some individuals inherit a tendency for weak arches. Additionally, obesity places excess strain on the feet, weakening the arch over time. Other causes include injuries or conditions that damage the tendons supporting the arch, such as posterior tibial tendon dysfunction. Chronic conditions like diabetes and rheumatoid arthritis can also contribute to the loss of the arch. If you have flat feet, it is suggested that you are under the care of a podiatrist who can offer you comfort options and help you to manage this condition.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Steven Shlonsky from Louisville, Kentucky. Dr. Shlonsky will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Louisville, KY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.